Uterine Fibroids, Non-Cancerous Tumors
Uterine fibroids are present in one out of every four or five women over the age of 35. Also called myomas, fibromyomas or leiomyomas, they can appear on the inside or outside lining of your uterus, or within its muscular wall. They usually develop from a single smooth muscle cell that continues to grow.
You may have a single fibroid or several. They can range from grapefruit to the size of a tiny pea. Although most fibroids remain small, their growth can be unpredictable. Some grow slowly, and others may grow very quickly. Most of the time, however, fibroids aren’t dangerous. They aren’t associated with an increased risk of uterine cancer and almost never develop into cancer.
Fibroids can require emergency treatment if they cause sudden, sharp pelvic pain. But this is a rare occurrence. In general, fibroids cause no problems and seldom require treatment. Drug therapy and surgical procedures can be used to shrink or remove fibroids if they do cause discomfort or troublesome symptoms.
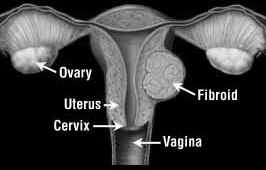 |
Fibroids can develop on the inside or outside lining of your uterus or within its muscular wall. Uterine fibroids are non-cancerous tumors of the uterus that appear during your childbearing years.
|
Signs and Symptoms of Fibroids
If you have uterine fibroids, you may not know it. At least half of all women with fibroids have no symptoms. In fact, most fibroids are discovered during a routine pelvic exam or during prenatal care. The most common symptoms of fibroids include:
- Abnormal menstrual bleeding — heavier or more prolonged than normal
- Pain in your abdomen or lower back
- Pain during sexual intercourse
- Symptoms of anemia due to heavy menstrual blood loss
- Difficult or frequent urination from the fibroid pressing on your bladder
- Pelvic pressure
- Infertility or miscarriage
- Constipation
Causes
It’s not clear why fibroids occur, although heredity seems to play a role. You're more likely to develop fibroids if other women in your family have them.
Hormonal factors seem to control fibroid growth, especially the production of the female hormone estrogen. Fibroids tend to grow during your reproductive years and may expand rapidly during pregnancy when your estrogen levels are very high. They generally shrink after menopause as estrogen levels decline. Other hormones, such as progesterone, also may affect fibroid growth.
Treatment
With fibroids that don’t cause symptoms, your doctor may suggest a wait-and-see approach. You may need regular follow-up visits and sometimes ultrasound exams to monitor the size of the fibroids.
If symptoms do develop, your doctor may recommend one of the following treatments:
Drug therapy
Oral contraceptives may help control heavy menstrual bleeding. The hormonal treatment danazol (Danocrine) also may be useful to control excessive menstrual flow. However, these therapies don’t control fibroid growth. Other drugs, known as gonadotropin-releasing hormone (Gn-RH) agonists (Lupron, Viadur, others) may be used to shrink fibroids by reducing the amount of estrogen in your body. This form of drug therapy is not a long-term solution, but may be used as a preparation for surgery. Unfortunately, Gn-RH agonists cause all of the symptoms of real menopause — including hot flashes, mood swings, headaches, vaginal dryness and bone loss. If you need prolonged treatment, your doctor can add other medications to reduce your menopausal symptoms. Fibroids often return after drug therapy is discontinued. Most medications for uterine fibroids are used only as temporary treatment in anticipation of menopause or surgery.
Surgery
Sometimes you may need surgery to remove a fibroid. One option is myomectomy, a surgical procedure in which only the fibroids are removed and your uterus is left intact. This is an important option if you're considering having children. The other surgical option is hysterectomy to remove your uterus. This is the most common effective approach, but needs to be done only when fibroids cause problems. Hysterectomy has a lower rate of complications than myomectomy and is a permanent solution for fibroids. Following myomectomy, fibroids return in about 10 percent of cases.
In the last 10 years, less invasive surgical techniques, such as hysteroscopic or laparoscopic removal of fibroids, have been developed. In these procedures surgeons use a long, thin instrument equipped with a light and video camera to see the area being treated on a video monitor. With hysteroscopic surgery the instrument or scope is inserted through your vagina and cervix into your uterus. In laparoscopic surgery, the scope is inserted through a small incision just below your navel and special instruments are used to remove the fibroids. With these techniques you'll likely heal more quickly and have little or no scarring. But they’re only an option if your fibroids are small and the chance of new fibroid development is high. Since small fibroids often require no treatment, laparoscopic surgery is rarely needed.
Uterine fibroid embolization
This non-surgical, minimally invasive procedure may be another option for some women who want to avoid surgery. It’s designed to shrink fibroids by cutting off the blood supply that feeds them. During the procedure, a doctor — typically a radiologist — uses X-ray images to guide a thin tube (catheter) through an artery in your leg to arteries in your uterus that feed fibroids. Once the catheter is in place, the doctor inserts tiny particles of plastic or gelatin through it to block blood flow inside the fibroids. Without blood supply, the fibroids shrink or disappear over time.
Fibroid embolization has been used for years to treat heavy bleeding after childbirth, but it’s relatively new for the treatment of fibroids. Studies have shown that about 85 percent of women who have the procedure report significant or complete relief of pain and other symptoms of fibroids. Fibroid embolization usually requires a hospital stay of one night, and most women experience cramping for a few hours to days after the procedure. The procedure carries a slight risk of injury to the uterus from decreased blood supply or infection. In addition, a few women have had their menstrual periods stop after fibroid embolization. Studies about getting pregnant after having this procedure aren’t complete. It’s also unclear whether uterine fibroids will return after this procedure. The long-term effects of fibroid embolization require more research.
Hearing the words fibroid tumors from your doctor could prompt a variety of reactions. The word tumor alone might spark fears that you have cancer. You might worry that you'll be unable to bear children. On the other hand, you could be relieved to know the reason for your prolonged, heavy menstrual bleeding. If fibroids led to your mother's hysterectomy, surgical removal of the uterus, you might believe that's your destiny, too.
Don't jump to conclusions. Fibroids are non-cancerous tumors that grow slowly and usually require no treatment. With this in mind, even if they cause symptoms, you still have a variety of treatment options.
We've provided informative documentation to what we believe to be a safe and effective natural alterative to prescribed medication for the treatment of fibroids. The key focus in the next section is on Anti Fibrosis.
Vitalzym Enzyme
|
